Empowering the Quintuple Aim: Embracing an essential architecture
As the industry faces new challenges and incentives, it needs to move to a digital-first, data-first, platform-based, human-centric architecture.

The healthcare industry has been facing mounting challenges, including rising costs, access disparities, workforce burnout and fragmented care delivery, which call for urgent solutions.
Increasing investments, inefficiencies and preventable errors contribute to ballooning costs, while fragmented care delivery leaves patients having to navigate these disjointed systems. With this comes the Quintuple Aim as a transformative framework that emphasizes health equity, as its fifth aim advocates for streamlined processes, patient-centered care, improved health of communities, sustainable models for care teams and equitable access to care for all.
Embracing a digital-first, data-first, platform-based, human-centric architecture is essential for realizing the Quintuple Aim’s vision.
Building blocks of the architecture
Here are some key components of this approach.
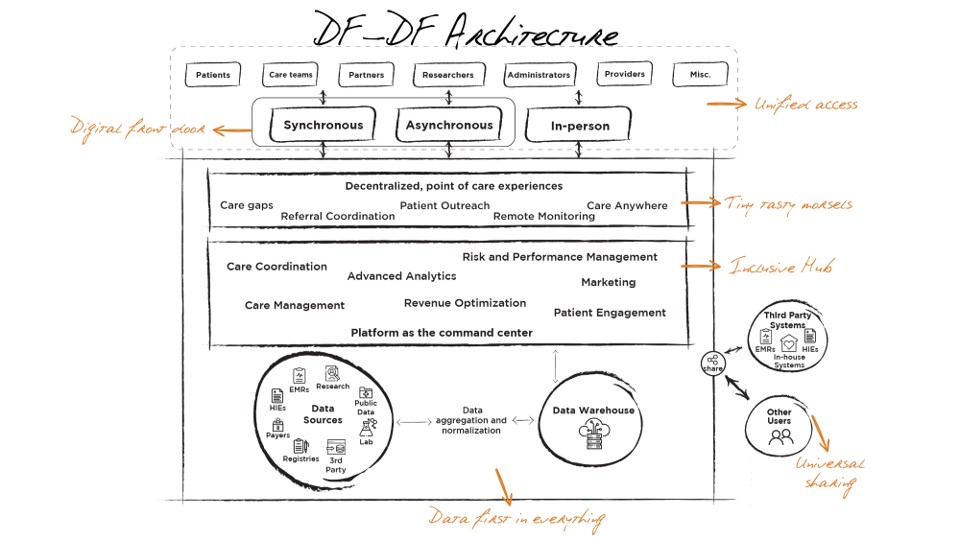
Data-first in everything. The architecture’s foundational and most critical structure is the backend tier that puts data-first in everything that architecture enables. Data is aggregated, cleansed, normalized, prepared and stored in a scalable, extensible data warehouse, regardless of source, size, type, location or format. Centralizing all data assets with a unified schema is essential to enabling the DF-DF architecture.
Platform as an inclusive hub. The operating system for the architecture is a technology-enabled platform that functions as a command center, bringing together all the functional experiences that drive end-user experiences and value-based care outcomes. This layer is the bedrock for core population health management, integrating all care coordination, patient engagement, advanced analytics, revenue optimization, risk and performance management functions in an inclusive, intuitive design.
Unified access. After the platform brings it all together as the hub, the next component is the need to unify access for all stakeholders – patients, care teams, physicians, administrators, partners, researchers and other authorized users. A key strategy to unify access is to enable a digital front door that co-exists with the in-person touchpoints. The digital front door should encompass both synchronous and asynchronous modalities, and work in harmony with in-person experiences like office encounters or home visits.
Tiny tasty morsels. The architecture's key objective is to empower “Care Anywhere” models that decentralize care delivery actions across all points of care. By enabling simple, rich, meaningful and actionable workflows such as care gap closure, referral coordination, patient outreach, remote monitoring and so on, these tools or “tiny, tasty morsels” help stakeholders focus on the right patients at the right time for the right reasons.
Universal sharing. A core principle of the architecture is to enable unlimited, unfiltered, secure, lossless and complete sharing of data, insights, and access to other valid third-party sources and users. This enables a symbiotic ecosystem to come together and drive better population health outcomes.
Benefits of the architecture
There are multiple benefits to this form of architecture.
Empower quintuple AIM. Lower costs of care, better care for the patient, improved health of communities, sustainable service model for care teams and equitable access to care for all.
Drive continuous process improvement. Bidirectional feedback loops enable the exchange of insights and information between patients and providers, improving care delivery and outcomes.
Integrate value-based care with traditional fee-for-service models. Shift focus from the volume of services provided to the quality and outcomes of care, incentivizing healthcare providers to deliver high-value, cost-effective care.
Comprehensive integration with anytime, anywhere access. Integrate patient data from disparate sources into a comprehensive and cohesive view, avoiding navigation between multiple windows and simplifying care processes.
Prepare for the future of medicine with more personalized care. With a better understanding of population health, individual care can be amplified through tailored interventions and proactive health management strategies.
As organizations shift from fee-for-service to value-based care models, leveraging interoperability platforms becomes increasingly crucial. With digital tools and data analytics capabilities, organizations can focus on what they do best – providing quality patient care.
By embracing the DF-DF, platform-based, human-centric architecture, healthcare organizations can navigate healthcare delivery complexities, deliver more effective care and improve global health outcomes. This transformative approach, aligned with the Quintuple Aim, equips providers with the tools needed to deliver patient-centric, personalized care experiences, address health equity and access challenges, and foster sustainable healthcare systems.
Jessica Marette Robinson is chief platform officer for The Garage In.