How technology can boost operational efficiency, reduce burnout
Artificial intelligence has the potential to predict and manage missed care opportunities, thus reducing cost and improving everyone’s experience.
The U.S. healthcare industry is facing a critical staffing shortage that shows no signs of improving. This shortage spans a range of healthcare positions, according to the Bureau of Labor Statistics. The agency projects that there may be a shortage of nearly 200,000 nurses by 2031, and that openings for home health aides and personal health aides will increase by 37 percent by 2028.
However, the most significant impact of this staffing shortage could be the shortfall in the number of physicians, with a report from the Association of American Medical Colleges (AAMC) estimating a shortage of as many as 124,000 physicians by 2034. In the same report, AAMC notes that the shortage of radiologists and other specialists could exceed 35,000.
More than 80 percent of health systems are reporting shortages in their radiology departments, a trend that is likely to continue during the next decade. These shortages are being driven by aging radiologists leaving the profession, with one estimate noting that of the nearly 21,000 radiologists involved in patient care, more than half are older than 55.
In addition, worker burnout is endemic to the broader healthcare profession. This is concerning and has implications for the future of innovation in the space, with the Centers for Disease Control and Prevention noting that the number of imaging studies being done increases by as much as 5 percent annually, while radiology residency positions are growing by only about 2 percent.
Minimizing missed care opportunities
Compounding the challenges of staffing shortages is the problem of missed care opportunities (MCO), which occur when a patient misses an appointment, fails to schedule a follow-up or is late. In radiology, studies indicate that an MCO – an imaging appointment that is scheduled but not performed, for example – can have a ripple effect, potentially delaying proper diagnosis and treatment, which could lead to increased morbidity and mortality.
While the reasons behind these no-shows are complex and may result from socioeconomic or logistical barriers – or even just forgetfulness – health systems bear the responsibility to help ensure that patients are making it to their appointments and that there are no unavoidable gaps in care.
The burden of these MCOs can include a discontinued care process, longer waiting time for appointments and an increase in admissions for services in the emergency department. In addition, missing and rescheduling an appointment also can negatively impact access to care for other patients, creating dissatisfaction among patients and healthcare providers through suboptimal care results.
For health systems, MCOs also represent lost revenue. One study in a vascular laboratory found that a no-show rate of just 12 percent results in a gross loss of $89,107 annually. However, a study demonstrated that reducing that rate to 5 percent could prevent revenue losses by $51,769. Clearly, there are incentives to reduce the impact of MCOs, and new technologies may offer a viable solution.
Technology’s role in countering challenges
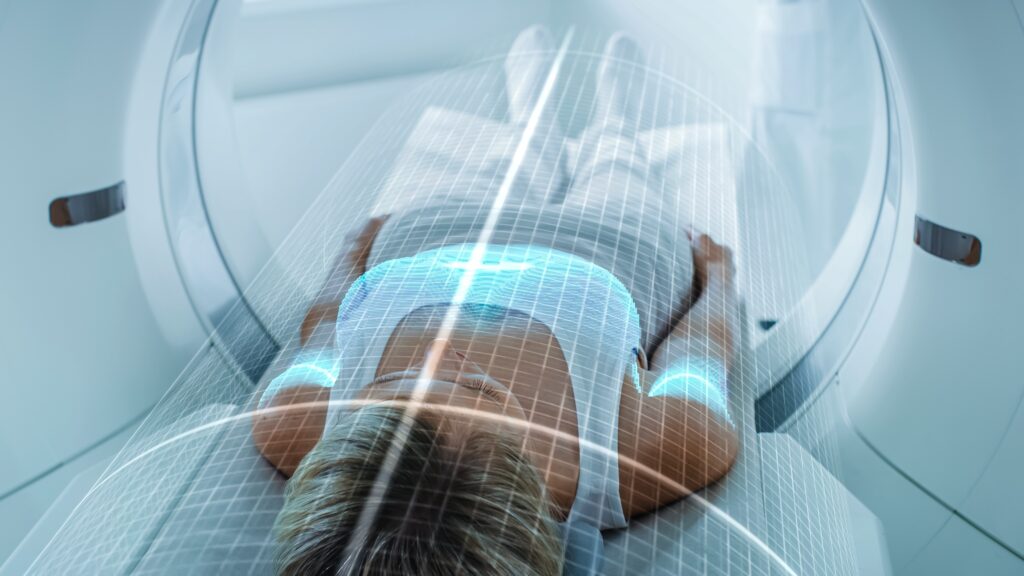
New technologies may offer a solution to help offset these shortages. From automating many processes to decreased imaging time and vastly improved imaging quality, emerging technologies offer the promise of freeing up radiologists to better focus their time on patient care.
The emergence of generative artificial intelligence (AI) and its ever-growing role in healthcare – particularly in imaging – may be one solution to help address these issues, as well to reduce the burden of administrative work that radiologists currently face.
With more than 80 percent of all hospital and health system visits including at least one imaging exam per patient and demand for imaging services continuing to rise, AI can play a critical role in overcoming the challenges of staff shortages and limited resources. However, it will be increasingly important for health systems to collaborate with trusted organizations to achieve the full benefits of AI in imaging.
Collaborating to boost operational efficiency
For health systems, taking concrete steps to utilize AI to predict MCOs and, consequently, increase operations effectiveness and productivity will be critical.
For example, Mass General Brigham recently deployed an AI algorithm to help increase operational effectiveness and productivity. The hospital is exploring the use of AI across a broad range of diagnostic and treatment paradigms to support each patient’s journey, from admittance through discharge. Radiology teams have deployed a digital imaging tool that helps optimize scheduling, reduce costs and free providers from administrative burden, freeing up more time for the clinician-patient relationship. In preliminary tests at one location in the system, the algorithm was able to predict the MCO correctly, at rates from 67 percent to 96 percent, with limited false positives.
In response to staffing shortages, collaborations leveraging AI and machine learning technologies have the potential to help alleviate physicians’ administrative burdens, resulting in less burnout and enabling them to spend more time with patients, which in turn may lead to better outcomes. These types of collaborations can usher in unprecedented healthcare advancements, bringing together hospitals, data sets, and clinical and technical minds to help solve several problems the healthcare field is currently facing.
The ability to predict MCOs and late arrivals with a high degree of accuracy could help increase flexibility and streamline administrative operations, improve patient satisfaction and better accommodate urgent care, inpatients or walk-in appointments. The use of AI to effectively address and overcome administrative barriers to care is a significant development, and there is growing hope that successful collaborations will drive further innovation in the industry focused on improving patient care and, equally important, the provider experience.
Parminder Bhatia is chief AI officer at GE HealthCare, responsible for leading the integration of artificial intelligence into the development, manufacturing and operation of medical devices, as well as for overseeing the implementation of artificial intelligence technologies to improve patient care, operational efficiency and outcomes.