How to build provider networks and contracts in specialty value-based care
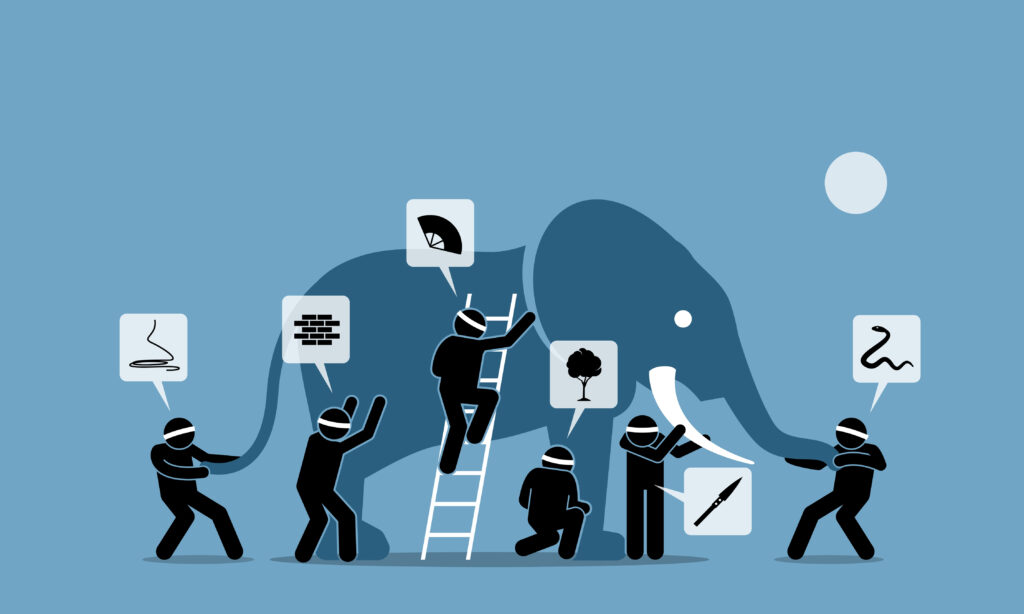
Sharing information among providers involves well-strategized approaches to ensure all data reaches those who need it, when they need it.
The first installment of this series explored the financial complexities of specialty value-based care and highlighted innovative models designed to address those challenges. From bundling payments to advanced episode-based reimbursement strategies, the focus was on aligning financial incentives with high-quality outcomes while mitigating risk.
Building on that foundation, this article delves into the mechanisms that enable effective implementation — network development, risk contracting and provider enablement.
Specialty care often drives the bulk of healthcare spending, making it a prime target for transformation in value-based arrangements. To realize the promise of value-based care, organizations must create scalable frameworks that integrate high-performance networks, transparent payment models and data-driven insights.
High-performance networks as a foundation
At the heart of any successful specialty value-based care model is a carefully curated provider network. High-performance networks bring together providers who demonstrate superior quality and cost-efficiency, ensuring that patients receive the best possible care without unnecessary expenditures.
Developing these networks often requires a tiered approach.
Tier 1: Contracted specialty providers . These are independent specialists participating in value-based agreements, focusing on outcomes and cost accountability.
Tier 2: Fee-for-service partners. These are providers under traditional reimbursement models to fill gaps and ensure geographic coverage.
Tier 3: Wraparound networks: Virtual care organizations and Centers of Excellence to augment local and national reach, providing flexible care delivery models that accommodate diverse patient needs.
By blending these tiers, organizations can create networks that balance broad access with a focus on value, giving payers and patients confidence in their ability to deliver effective care.
Aligning incentives with risk contracting and payment models
While network design establishes the structure, payment models define the financial framework that incentivizes value-based performance. Advanced alternative payment methodologies, such as bundled payments and condition-specific episodes of care, align provider reimbursement with quality and efficiency goals.
These models rely on the following factors.
Data-driven design. Payments should be anchored in objective metrics, leveraging national benchmarks and external validation.
Transparency. Fixed, predictable pricing ensures stakeholders understand cost structures and expected outcomes.
Flexibility across care settings. Consistent methodologies spanning inpatient, outpatient and ancillary services reduce variability and streamline administration.
To operationalize these strategies, risk-bearing entities with risk-contracting engines play a critical role. These entities systematically analyze claims and eligibility data to define and track episodes of care, attributing services and costs to specific providers. They also create feedback loops that enable organizations to monitor performance and refine contracts as needed.
Tools for success in provider engagement
Engaging and supporting providers is crucial to driving adoption and sustaining performance in value-based models. Provider enablement platforms offer the tools needed to manage risk and improve outcomes. These include the following.
Real-time decision support. Dashboards and analytics help providers monitor episodes, identify gaps and intervene early to prevent complications.
Simplified administrative processes. Automation powered by machine learning and artificial intelligence reduces the burden of authorizations and processing.
Actionable insights. Reporting capabilities allow providers to benchmark their performance, track cost trends, and make data-informed adjustments.
With these capabilities, providers can focus on delivering high-quality care rather than navigating administrative hurdles, leading to better patient experiences and stronger financial performance.
Geographic expansion and specialty growth
For value-based care models to succeed, they must scale efficiently across markets and specialties. A phased approach enables organizations to prioritize high-impact specialties — such as cardiology, oncology, orthopedics and gastroenterology — before expanding to additional areas.
Key elements of scaling include the following.
Network adequacy. This helps ensure coverage through a mix of direct contracts and wraparound networks.
Contracting roadmaps. Sequencing provider outreach, negotiations and legal reviews can help meet growth targets.
Specialty prioritization. Focusing first on specialties with the highest spending and growth potential before broadening to secondary areas.
By establishing clear processes and timelines, organizations can accelerate their impact while maintaining quality and cost control.
Sustaining specialty care transformation
Infrastructure is critical to operationalize value-based care — from building high-performance networks to aligning incentives and equipping providers for success. However, transformation doesn’t end here.
The third article in this series will explore how organizations can sustain and expand their impact by embracing continuous innovation. It will discuss the role of predictive analytics, artificial intelligence and patient engagement technologies, among other innovations, in driving long-term performance and delivering exceptional value.
As we move forward, the goal remains clear — to build systems that not only manage costs but also elevate outcomes, ensuring that specialty care becomes a cornerstone of sustainable value-based healthcare.
Crystal Crider, DHA, MHA, FACHE, eFACHDM, is a vice president of product at Enlace Health and holds adjunct instructor positions at both UCF and AUM.
