Why driving authentic value is key to improving patient experience
Patients’ key goals for care often include personal, psychological or relational factors – and that’s not how organizations typically define value-based care.
Many initiatives have aimed to revolutionize healthcare delivery, and the transformation journey has been challenging. While the evolution towards value-based healthcare offers optimistic possibilities, reform efforts have disproportionally focused on the change of reimbursement methods.

The core of value-based care lies in providing high-quality care at the most affordable cost, prioritizing patient health outcomes over the quantity of services provided.
Patients, as consumers, seek transformation that provides authentic value, which prioritizes their experience and desired health outcomes, in relationship to financial concerns. To achieve authentic value, health and care leaders must focus on what matters most to patients. We must build our models that reduce burdens for organizations and care teams as they strive to deliver on the needs and expectations of patients.
This shift represents a dramatic change for health and care delivery organizations. Achieving it necessitates a dedicated investment, including building a human-centered culture, developing an integrated data strategy and leveraging relevant technological innovations.
What is authentic value-based care?
The value-based healthcare (VBC) movement was designed to transform healthcare delivery by incentivizing healthcare providers to deliver the best possible care at the lowest cost, focusing on improving the quality and efficiency of care rather than the volume of services provided. The foundational book, “Redefining Health Care: Creating Value-Based Competition on Results,” defined value by measuring patient health outcomes in relationship to cost.
Efforts toward a value-based transformation often emphasize cost, process and efficiency outcomes. While financial concerns remain critical for healthcare reform, authentic value prioritizes the experience and health outcomes that matter most to patients, with cost reduction as an ancillary effect.
Patients’ goals often include personal, psychological or relational factors. For example, a study entitled "Understanding What Matters Most to Patients in Acute Care in Seven Countries, Using the Flash Mob Study Design," asked patients what mattered most to them during the first 24 hours of acute hospital admission. Overall, their goals focused on achieving good health, returning home and receiving a diagnosis.
However, some 50 percent of patients said they do not believe their providers knew what mattered to them. Participants expressed motivations related to being with family and friends, resuming normal life, being more comfortable, taking care of others, feeling less anxious or insecure and, of course, receiving treatment.
To improve experience and health outcomes, provider organizations need to update models to measure value in ways that matter to both patients, clinical care experts and healthcare delivery organizations.
In the book “Competing Against Luck,” the authors argue that when a consumer buys a product, they aim to make progress and “get a job done.” If their goals are achieved, then they “hire” the product again and look for something else. When the framework is applied to healthcare organizations, the achievement of health outcomes creates a natural alignment around shared goals and mutual benefit for achieving them even more so, compared with other industries.
To remain competitive, healthcare leaders must communicate and work together with patients and their workforce to understand what quality care means to them, rather than making assumptions or relying on traditional, less inclusive measures.
Defining patient experience
The Agency for Healthcare Research and Quality (AHRQ) describes patient experience as the range of interactions that individuals and families have with the healthcare system, and, as such, it is an integral component of healthcare quality.
Many factors influence our healthcare experiences (Figure 1), including interactions with healthcare providers, the accessibility and convenience of care, the physical environment, and the overall emotional and psychological impact of these encounters.

Although patient experience is widely recognized as an important quality measure, definitions are often diverse and dependent on the perspective of the one creating the definition. The article, Understanding the Patient Experience: A Conceptual Framework, published by The Journal of Patient Experience, highlights the evolution of patient experience and the many definitions that persist.
Central to the understanding of patient experience is the differentiation between the terms satisfaction, experience and engagement. Often used interchangeably by healthcare professionals, Figure 2 offers a simplified explanation of the terms, based on evidence-based materials shared by AHRQ.
Experience refers to “whether something that should happen in a healthcare setting (such as clear communication with a provider) actually happened or how often it happened.”
Satisfaction, on the other hand, is about whether a patient’s expectations about a health encounter were met. Two people who receive the exact same care, but who have different expectations for how that care is supposed to be delivered, can give different satisfaction ratings because of their different expectations.”
Engagement refers to “the inclusion of patients and family members as active members of the healthcare team and collaborative partnerships with providers and provider organizations.”
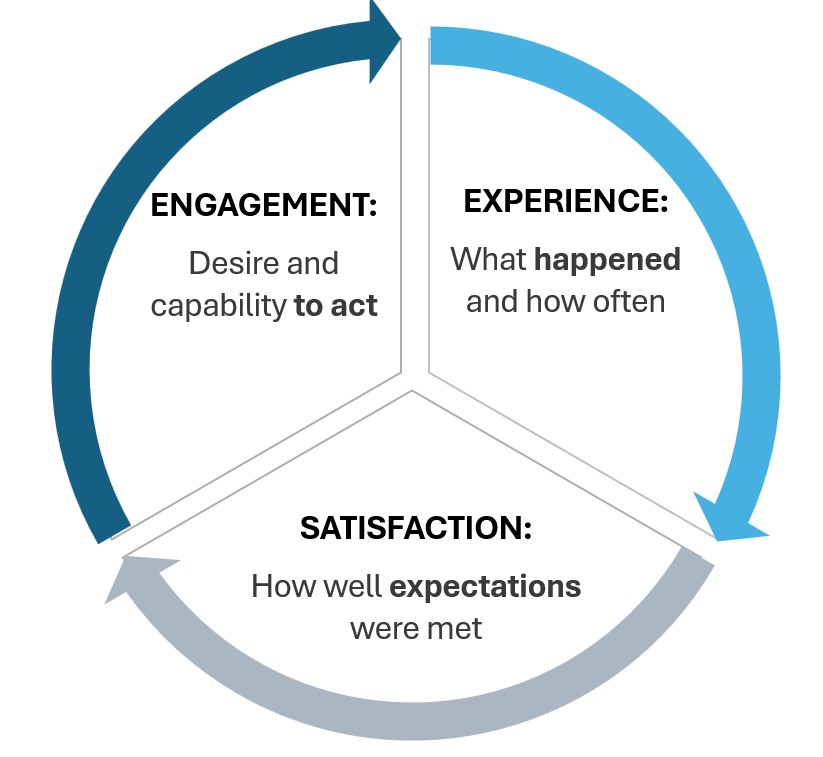
The reciprocal relationship between these elements can support better health outcomes, which often translate to lower costs in a value-based arrangement.
Leveraging experience to drive authentic value
The reciprocal relationship between experience, satisfaction and engagement influences our ability to deliver authentic value. Many studies have delved into patient experience improvement efforts, aiming to focus on what matters most to patients. (Visit The Journal of Patient Experience for free access to hundreds of evidence-based articles.)
A recent VBC framework published in Academic Medicine outlined the importance of understanding the shared health needs of patients as a core strategic element. We can then advance solutions to drive and measure health outcomes, to integrate teams and to expand partnerships.
The authors advocate for a shift beyond a focus on cost or experience to instead prioritize individuals’ needs, such as capability, comfort and calm.

Improving patient experience has a wide range of aligned benefits across various aspects of health and care, including advantages for patients, clinical teams and systems (Figure 3).
Benefits for patients
Benefits for clinical teams
Benefits for healthcare systems
When we determine value with patients – not for them – efforts focus more on achieving meaningful outcomes. For healthcare organizations, this means consistently delivering on the promise to help patients reach their health goals, which builds trust, engagement and loyalty.
This approach requires organizations to continuously improve and design experiences that create high-value interactions. By doing so, organizations can foster authentic relationships and unlock new potential for achieving health outcomes.
Measuring authentic value
Patient-reported outcome measures (PROMs) are tools used to capture patients' perspectives on their health status, including symptoms, functional status and quality of life.
Patient-reported experience measures (PREMs), on the other hand, focus on patients' experiences with healthcare services, such as communication with providers, wait times and overall satisfaction with care.
A recent article on “Driving Value Through Standardized Measurement of Patient Reported Outcomes,” outlined the domains of outcomes and experience measures. PROMs often assess physical, social, emotional and cognitive function, as well as domains health literacy, side effects and adherence. PREMs often assess treatment, technology and communication experiences, as well as satisfaction and engagement.
Integrating PROMs and PREMs into clinical workflows is essential to streamline the process and minimize the burden on both patients and care teams. By embedding these measures seamlessly into routine care, consistent and reliable data collection can be ensured without adding extra steps for anyone involved. This approach not only enhances the quality of care but also fosters a more efficient and patient-centered healthcare system.
Taking steps to drive authentic value
Inspired by the strategic framework of Teisberg and colleagues, here are some initial steps toward a strategy for authentic value.
While concerns around cost remain central to sustainability and healthcare reform, an authentic value-based model represents a human-centered approach by intentionally designing care experiences that strengthen engagement and achieve mutual benefits and outcomes.
Laura Cooley, PhD, is editor-in-chief of the Journal of Patient Experience, in which she advocates for improved health and experience outcomes through evidence-based research and practice. Rachel Biblow is a healthcare executive who relentlessly pursues better health, experience and business outcomes.
Meet the authors at The Patient Experience Symposium in Boston September 16 to 18.