Why interoperability plays a key role in improving care, efficiency
Achieving the Quintuple Aim requires seamless communication among technologies, streamlined processes and cross-industry collaboration.
Effective interoperability ensures that healthcare providers have timely access to comprehensive patient information, thereby facilitating informed decision-making and personalized treatment plans.
Experts see interoperability playing an increasingly important role in achieving the Quintuple Aim – improving patient experience, enhancing care team well-being, achieving better outcomes, reducing costs and ensuring equitable access to care. These goals highlight the need for seamless communication among technologies, streamlined processes and cross-industry collaboration. As healthcare evolves, interoperability remains a key focus for innovation and collaboration.
The importance of seamless data exchange is part and parcel of the Trusted Exchange Framework and Common Agreement, otherwise known as TEFCA. The federal initiative is considered one of the most important initiatives in interoperability today.
The role of TEFCA goes beyond just patient treatment. “TEFCA also aims to include individual access services, payment, healthcare operations, public health exchange and public benefits determination,” says Steven Lane, MD, chief medical officer at Health Gorilla.
In an HDM article, Lane notes that while TEFCA holds great promise, it faces challenges in achieving clinician adoption. Despite the benefits of interoperability, getting clinicians to embrace new systems and workflows can be difficult. Lane notes, adding that, "The key is bringing this exchanged data into workflow and making it actionable."
The imperative of interoperability
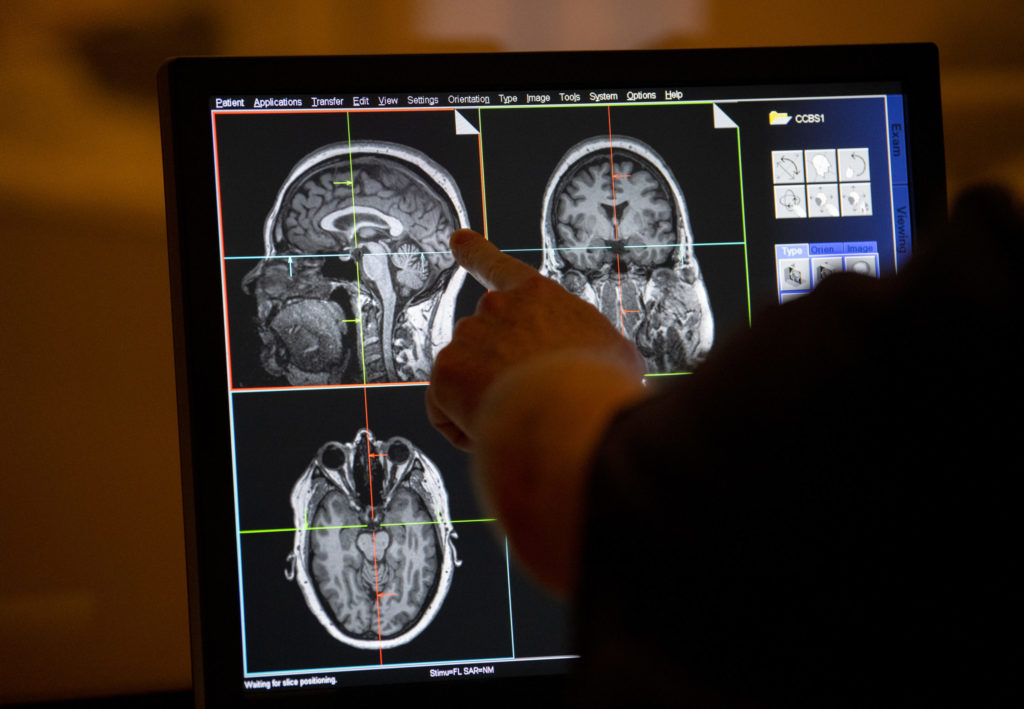
At its heart, interoperability refers to the capability of different health information systems, devices and applications to access, exchange and cooperatively use data in a coordinated manner. This functionality is essential for providing clinicians with a holistic view of a patient's health history, which is critical for accurate diagnoses and effective treatments.
As highlighted in a recent article, "Access to accurate, real-time data is critical for improving clinical outcomes. Healthcare providers need a complete view of their patients’ health histories, diagnoses, and treatments to make informed decisions," writes Michael Lawrence in his article in Health Data Management.
Insights from healthcare leaders
Healthcare professionals recognize the challenges and are actively working towards enhancing interoperability within their organizations.
Herat Joshi, a Fellow of the American College of Health Data Management, emphasizes the importance of foundational data quality and system integration. "We are focused on improving electronic health record integration and mentoring teams in AI governance,” Joshi explains. “Our approach underscores that innovation must rest on solid data, systems, and policies."
Similarly, Kimberly Montero, another ACHDM Fellow, underscores the necessity of continuous learning and adaptation.
"To ensure our teams remain adaptable, we’ve integrated ethical and compliance training into our core upskilling programs,” she says. “It’s not enough to know how to run a model — you have to understand what it means when that model fails."
While the push for interoperability aims to foster innovation and improve patient access to health information, it also raises concerns about data security and privacy. Enhancements in data sharing must be meticulously balanced with robust security measures to protect sensitive patient information.
As noted in a Health Data Management article, "Improvements in data sharing require giving patients more control over their data and ensuring the security of sensitive information." The flip side, however, is that wider access raises new vulnerabilities that can jeopardize overall system security.
Strategies for enhancing interoperability
To navigate the complexities associated with interoperability, healthcare organizations can adopt several strategic approaches.
Adoption of standardized protocols. Implementing widely accepted standards such as Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR) facilitates consistent data exchange across diverse systems.
Investment in advanced technologies. Leveraging technologies like blockchain can enhance data security and integrity, addressing critical concerns in data sharing.
Focus on semantic interoperability. Ensuring that exchanged data maintains its meaning across different systems is vital for effective communication and utilization, experts indicate.
Continuous staff training. Regular training programs for staff on the latest interoperability standards and technologies can facilitate smoother transitions and effective implementation.
Interoperability thus represents more than simply a technical challenge. Improving organizational readiness is essential to take full advantage of information availability, and both clinicians and patients have to be brought up to speed to safely access and incorporate digital information in modern care delivery.
